Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Cardiovascular Outcomes of Obesity According to Menopausal Status: A Nationwide Population-Based Study
- Bo Kyung Koo, Sang-Hyun Park, Kyungdo Han, Min Kyong Moon
- Endocrinol Metab. 2021;36(5):1029-1041. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1197
- 3,678 View
- 117 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We estimated the effect of obesity on the incidence of cardiovascular disease (CVD) and mortality in women according to menopausal status.
Methods
Women aged 40 to 69 years under routine health check-ups provided by the National Health Insurance Service in 2009 were followed up till 2018 (n=2,208,559).
Results
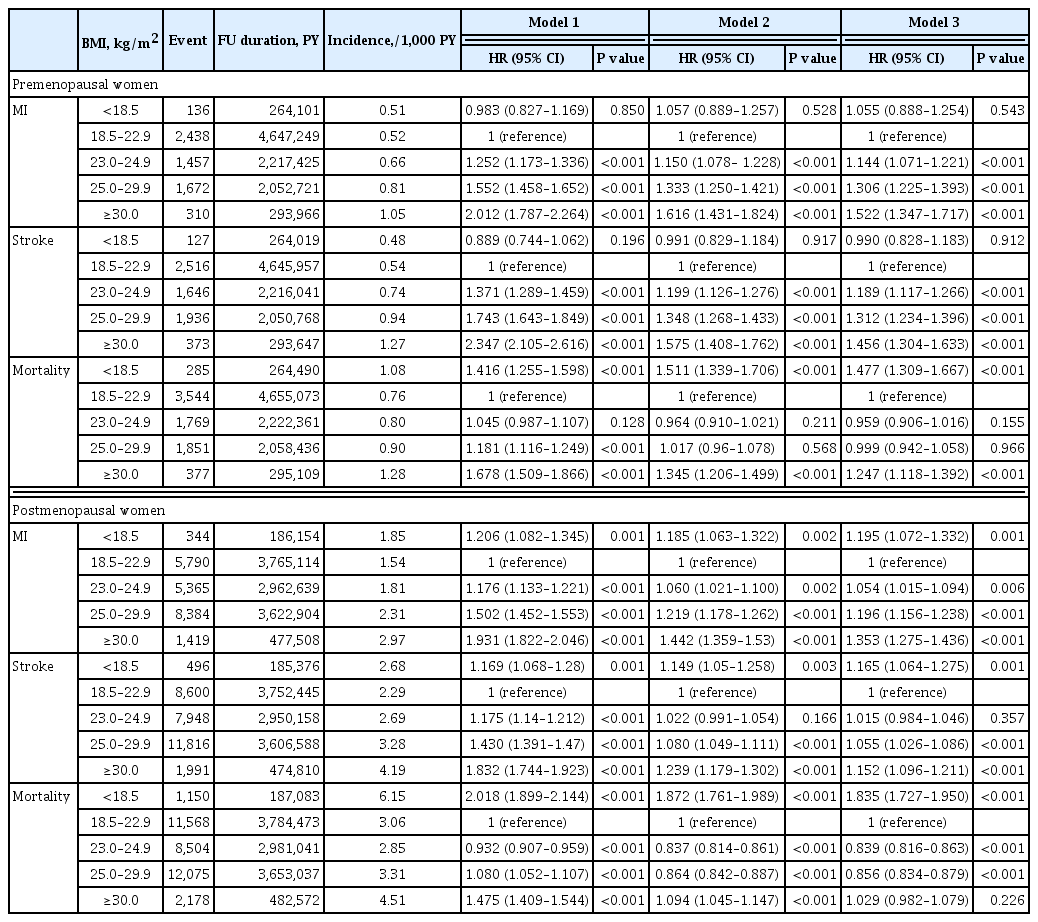
In premenopausal women, a significant increment of mortality rate was found in underweight and obesity class II (hazard ratio [HR], 1.48; 95% confidence interval [CI], 1.31 to 1.67; and HR, 1.25; 95% CI, 1.12 to 1.39) compared to normal body mass index (BMI); overweight and obesity class I did not affect mortality rate. In postmenopausal women, obesity as well as overweight status reduced the risk of mortality compared to normal BMI (HR, 0.86; 95% CI, 0.83 to 0.88; and HR, 0.84; 95% CI, 0.82 to 0.86). By contrast, there was a linear association between CVD and BMI above the normal range irrespective of menopausal status, which was attenuated in diabetic women.
Conclusion
The current study replicated the J-shaped relationship between BMI and mortality, being more prominent in the postmenopausal group. The risk of CVD was linearly increased as BMI was increased above the normal range irrespective of menopausal status. -
Citations
Citations to this article as recorded by- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension
Geetha Kandasamy, Thangamani Subramani, Gigi Sam, Mona Almanasef, Tahani Almeleebia, Eman Shorog, Asma M. Alshahrani, Amjad Hmlan, Atheer Y. Al Suhaym, Kousalya Prabahar, Vinoth Prabhu Veeramani, Palanisamy Amirthalingam
Frontiers in Cardiovascular Medicine.2024;[Epub] CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 45. CrossRef - The effect of menopause on cardiovascular risk factors according to body mass index in middle-aged Korean women
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Aysha Almas
PLOS ONE.2023; 18(3): e0283393. CrossRef - Low‐quality muscle mass rather than normal‐quality muscle mass determines fibrosis progression in biopsy‐proven NAFLD
Yun Kyu Lee, Bo Kyung Koo, Sae Kyung Joo, Dong Hyeon Lee, Heejoon Jang, Jee Won Chai, Myoung Seok Lee, Si Won Jang, Young Ho So, Jeong Hwan Park, Mee Soo Chang, Won Kim
Alimentary Pharmacology & Therapeutics.2023; 58(3): 322. CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Non-pharmacologic treatment for obesity
Bo Kyung Koo
Journal of the Korean Medical Association.2022; 65(7): 400. CrossRef
- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension

- Clinical Study
- Associations of Perirenal Fat Thickness with Renal and Systemic Calcified Atherosclerosis
- Bo Kyung Koo, Julie O. Denenberg, C. Michael Wright, Michael H. Criqui, Matthew A. Allison
- Endocrinol Metab. 2020;35(1):122-131. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.122

- 6,075 View
- 103 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background We investigated associations between perirenal fat thickness and atherosclerotic calcification in six different vascular beds.
Methods Using a community-based cohort (
n =3,919), perirenal fat thickness was estimated from computed tomography scans. It was classified as Q1 (the lowest quartile) to Q4 (the highest quartile) in each sex. Calcification in the carotid arteries, coronary arteries, thoracic aorta, abdominal aorta, iliac arteries, and renal arteries was evaluated.Results Perirenal fat thickness was associated with older age (
P <0.01) and a higher prevalence of obesity, hypertension, and dyslipidemia (P <0.01 for all). Perirenal fat thickness was independently associated with renal arterial calcification even after adjustment for age, sex, body mass index, hypertension, dyslipidemia, smoking history, and family history of heart diseases in first-degree relatives (odds ratio [OR] per quartile of perirenal fat thickness, 1.25; 95% confidence interval [CI], 1.09 to 1.44). Compared to Q1, the odds of renal arterial calcification in Q4 was about two times higher (OR, 2.05; 95% CI, 1.29 to 3.25). After adjustment for renal arterial calcification and atherosclerotic risk factors, the only other vascular bed where perirenal fat thickness showed a significant association with calcification was the abdominal aorta (OR, 1.11; 95% CI, 1.00 to 1.23;P =0.045).Conclusion Perirenal fat thickness was independently associated with vascular calcification in the renal artery and abdominal aorta.
-
Citations
Citations to this article as recorded by- Impact of Liver Transplantation on Adipose Tissue Compartments and Its Association With Metabolic Sequela
Ramzi Hassouneh, Sean Flynn, Steve Shen, Michael Tseng, Anh Tuan Bui, Jay Pham, Dan Park, Scott Matherly, David Bruno, Seung Lee, Vinay Kumaran, Vaishali Patel, Mark Muthiah, Amit Sharma, Mohammad Shadab Siddiqui
Transplantation.2024; 108(1): 235. CrossRef - High perirenal fat thickness predicts a greater risk of recurrence in Chinese patients with unilateral nephrolithiasis
Haichao Huang, Shi Chen, Wenzhao Zhang, Tao Wang, Peide Bai, Jinchun Xing, Huiqiang Wang, Bin Chen
Renal Failure.2023;[Epub] CrossRef - Development and validation of a preoperative nomogram for predicting the surgical difficulty of laparoscopic colectomy for right colon cancer: a retrospective analysis
Ao Yu, Yuekai Li, Haifeng Zhang, Guanbo Hu, Yuetang Zhao, Jinghao Guo, Meng Wei, Wenbin Yu, Zhibo Yan
International Journal of Surgery.2023; 109(4): 870. CrossRef - Perirenal Adipose Tissue Is Associated With Renal Dysfunction and Abnormal Hemodynamics in Patients With HFpEF
Eva M. Boorsma, Hidemi Sorimachi, Jozine M. ter Maaten, Dirk J. van Veldhuisen, Kazunori Omote, Naoki Takahashi, Jeffrey M. Testani, Tineke P. Willems, Adriaan A. Voors, Barry A. Borlaug
JACC: Heart Failure.2023; 11(10): 1463. CrossRef - Renal Compression in Heart Failure
Eva M. Boorsma, Jozine M. ter Maaten, Adriaan A. Voors, Dirk J. van Veldhuisen
JACC: Heart Failure.2022; 10(3): 175. CrossRef - The perirenal fat thickness was independently associated with serum uric acid level in patients with type 2 diabetes mellitus
Yuxian Yang, Yan Ma, Yanan Cheng, Yuechao Xu, Yuan Fang, Jing Ke, Dong Zhao
BMC Endocrine Disorders.2022;[Epub] CrossRef - Cardiorenal Fat: A Cardiovascular Risk Factor With Implications in Chronic Kidney Disease
Luis D'Marco, María Jesús Puchades, Nayara Panizo, María Romero-Parra, Lorena Gandía, Elena Giménez-Civera, Elisa Pérez-Bernat, Miguel Gonzalez-Rico, José Luis Gorriz
Frontiers in Medicine.2021;[Epub] CrossRef - Anti-Obesity Effects of a Prunus persica and Nelumbo nucifera Mixture in Mice Fed a High-Fat Diet
Jungbin Song, Jiye Kim, Hyo Jin Park, Hocheol Kim
Nutrients.2020; 12(11): 3392. CrossRef
- Impact of Liver Transplantation on Adipose Tissue Compartments and Its Association With Metabolic Sequela

- Clinical Study
- Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes
- Han Na Jang, Ye Seul Yang, Seong Ok Lee, Tae Jung Oh, Bo Kyung Koo, Hye Seung Jung
- Endocrinol Metab. 2019;34(4):382-389. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.382
- 4,994 View
- 143 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Conflicting results have been reported on the efficacy of insulin degludec/insulin aspart (IDegAsp) compared to basal insulin in type 2 diabetes. We investigated the effects of changing basal insulin to IDegAsp on glycemic control and sought to identify factors related to those effects.
Methods In this retrospective study of patients from three referral hospitals, patients with type 2 diabetes using basal insulin with hemoglobin A1c (HbA1c) levels less than 11.0% were enrolled. Basal insulin was replaced with IDegAsp, and data were analyzed from 3 months before to 3 months after the replacement.
Results Eighty patients were recruited (52.5% male; mean age, 67.0±9.8 years; mean duration of diabetes, 18.9±8.5 years; mean HbA1c, 8.7%±1.0%). HbA1c levels increased during 3 months of basal insulin use, but significantly decreased after changing to IDegAsp (8.28%±1.10%,
P =0.0001). The reduction was significant at 6 months in 35 patients whose longer-term data were available. Patients with a measured fasting plasma glucose (m-FPG) lower than their predicted FPG (p-FPG) by regression from HbA1c showed a significant HbA1c reduction caused by the change to IDegAsp, even without a significantly increased insulin dose. However, patients whose m-FPG was higher than their p-FPG did not experience a significant HbA1c reduction, despite a significantly increased insulin dose. Furthermore, the HbA1c reduction caused by IDegAsp was significant in patients with low fasting C-peptide levels and high insulin doses.Conclusion We observed a significant glucose-lowering effect by replacing basal insulin with IDegAsp, especially in patients with a lower m-FPG than p-FPG.
-
Citations
Citations to this article as recorded by- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience
Gökçen Güngör Semiz, İsmail Selimoğlu, Mehmet Emin Arayici, Serkan Yener, Abdurrahman Çömlekçi, Tevfik Demir
International Journal of Diabetes in Developing Countries.2023; 43(4): 544. CrossRef - Low fasting glucose‐to‐estimated average glucose ratio was associated with superior response to insulin degludec/aspart compared with basal insulin in patients with type 2 diabetes
Han Na Jang, Ye Seul Yang, Tae Jung Oh, Bo Kyung Koo, Seong Ok Lee, Kyong Soo Park, Hak Chul Jang, Hye Seung Jung
Journal of Diabetes Investigation.2022; 13(1): 85. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart (IDegAsp) in Type 2 Diabetes: Systematic Review and Meta-Analysis
Brenda C Edina, Jeremy R Tandaju, Lowilius Wiyono
Cureus.2022;[Epub] CrossRef - Comparing time to intensification between insulin degludec/insulin aspart and insulin glargine: A single-center experience from India
Rajiv Kovil
Journal of Diabetology.2022; 13(2): 171. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart Compared with a Conventional Premixed Insulin or Basal Insulin: A Meta-Analysis
Shinje Moon, Hye-Soo Chung, Yoon-Jung Kim, Jae-Myung Yu, Woo-Ju Jeong, Jiwon Park, Chang-Myung Oh
Metabolites.2021; 11(9): 639. CrossRef - Fear of Hypoglycemia in Adults with diabetes mellitus switching to Treatment with IDegAsp Co-formulation to Examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Drug Interactions.2021; 36(2): 129. CrossRef - Response: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Han Na Jang, Hye Seung Jung
Endocrinology and Metabolism.2020; 35(1): 194. CrossRef - Letter: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Sang Youl Rhee
Endocrinology and Metabolism.2020; 35(1): 192. CrossRef - Fear of hypoglycemia in adults with diabetes mellitus switching to treatment with IDegAsp co-formulation to examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Personalized Therapy.2020;[Epub] CrossRef
- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience

- A case of Paraganglioma Arising in the Transverse Mesocolon.
- Hong Il Kim, Bo kyung Koo, You Jin Lee, Jin Taek Kim, Young Min Cho, Kuhn Uk Lee, Seong Yeon Kim
- J Korean Endocr Soc. 2005;20(5):496-501. Published online October 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.5.496
- 1,624 View
- 17 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Herein, a case of a solitary primary paraganglioma arising in the mesentery, found in a hypertensive 70-year-old woman, who presented with nausea and postprandial abdominal discomfort, is reported. Ultrasonography and computed tomography showed a hypervascular mass abutting the second portion of the duodenum. An exploratory laparotomy revealed a 5.5 x 5.3 x 5cm sized mass in the mesentery of the transverse colon, which was histologically proven to be a paraganglioma. No intraoperative hemodynamic changes developed, and the postoperative course was uneventful. To our knowledge, this is the first case of a paraganglioma arising in the mesentery reported in Korea. Considering the unusual locations and the associated operative risk, it is necessary to rule out the possibility of a functioning paraganglioma in the preoperative differential diagnosis of an abdominal mass.
-
Citations
Citations to this article as recorded by- Mesenteric Lesions with Similar or Distinctive Appearances on CT
Hwajin Cha, Jiyoung Hwang, Seong Sook Hong, Eun Ji Lee, Hyun-joo Kim, Yun-Woo Chang
Journal of the Korean Society of Radiology.2019; 80(6): 1091. CrossRef
- Mesenteric Lesions with Similar or Distinctive Appearances on CT


 KES
KES

 First
First Prev
Prev



